Direct Care Workers In the Time of COVID-19
The past several weeks have brought stories of frontline, direct care workers who continue to support our most vulnerable community members despite COVID-19 related safety concerns, inadequate supplies, and ongoing questions about how to access essential services like child care. A workforce that’s projected to serve almost half of all adults 65 and older, home health aides, personal care aides, and certified nursing assistants have always been essential to the health and well-being of our communities. But in the midst of a public health crisis, these workers are literally saving lives by providing older adults with the day-to-day care they need.
Just as the current COVID-19 outbreak is spotlighting the value of these workers, it’s also exposing long-standing, systemic failings in how we support those who provide paid care to our older adults. Well before the current health crisis, the direct care workforce was plagued by low wages, poor benefits, and inadequate training. Now, in the middle of a public health epidemic, these preexisting vulnerabilities are creating dangerous cracks in our caring ecosystem.
| Hourly Wage Needed to Achieve Adequate Economic Security | Personal Care Aide Workforce Size & Median Wages | Home Health Aide Workforce Size & Median Wages | Nursing Assistant Workforce Size & Median Wages | |
| Total # Workers Throughout the State | — | 25,890 | 13,710 | 20,040 |
| Denver Metro | $19.81 | $11.78 | $12.31 | $16.21 |
| Fort Collins | $18.72 | $11.72 | $12.67 | $15.42 |
| Grand Junction | $17.59 | $10.85 | $11.99 | $13.56 |
| Pueblo | $16.16 | $11.08 | $11.31 | $14.65 |
Needed hourly wage from EPI and calculated based upon the needs of a single individual. Information on direct care worker wages and size from Careeronestop.
In response to COVID-19, state and federal policymakers are advancing meaningful supports for workers in the form of enhanced benefits, low-cost child care services, and better training and resources. However, as we analyze the impact of these policies, it’s important to do so with an eye toward ensuring they meet the needs of those — like direct care workers — who were already falling through the cracks.
Workplace Benefits
As seen below, prior to the outbreak of COVID-19, direct care workers were less likely to have access to essential workplace benefits, like health care and paid family, medical, and sick leave.
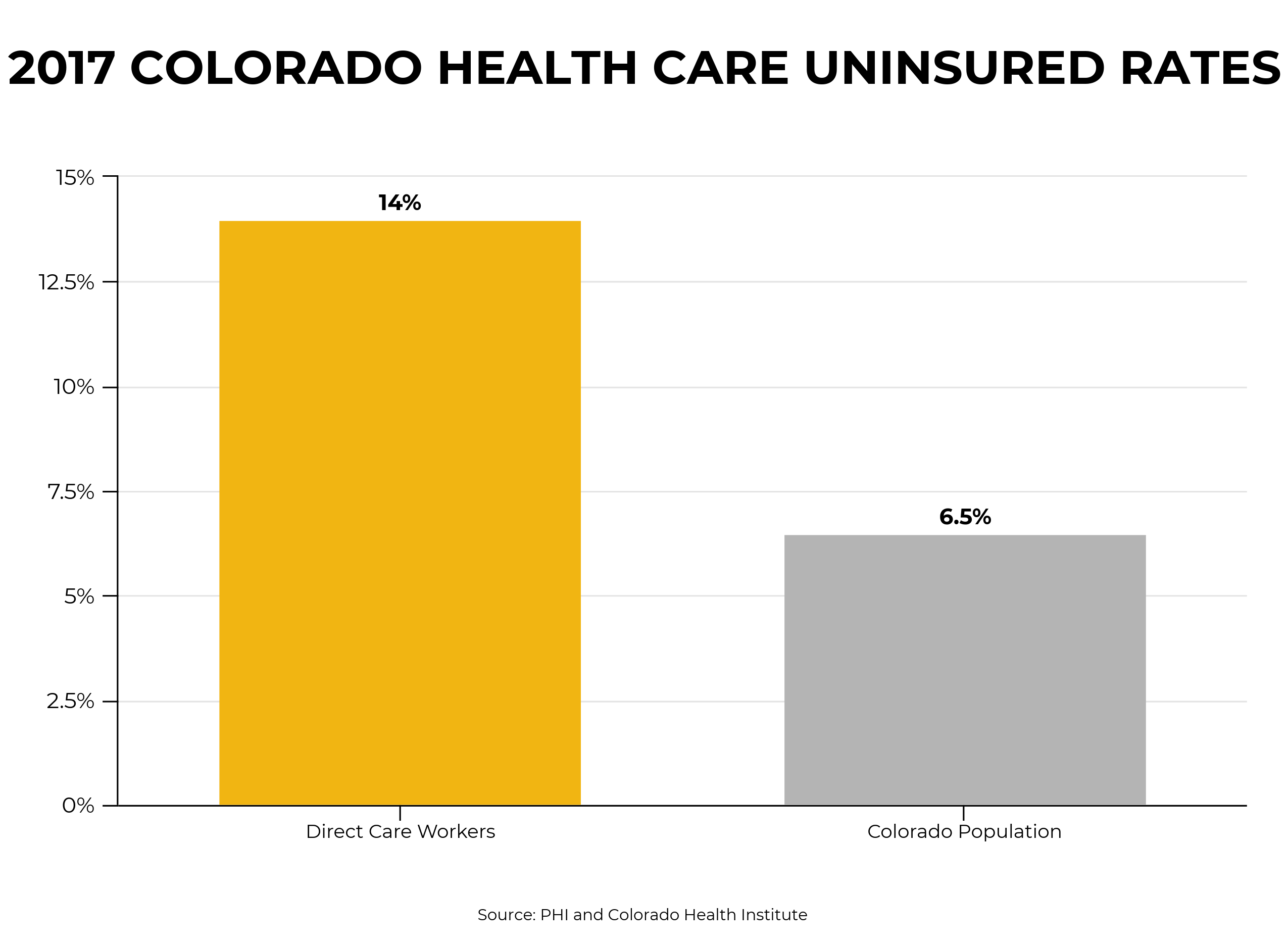
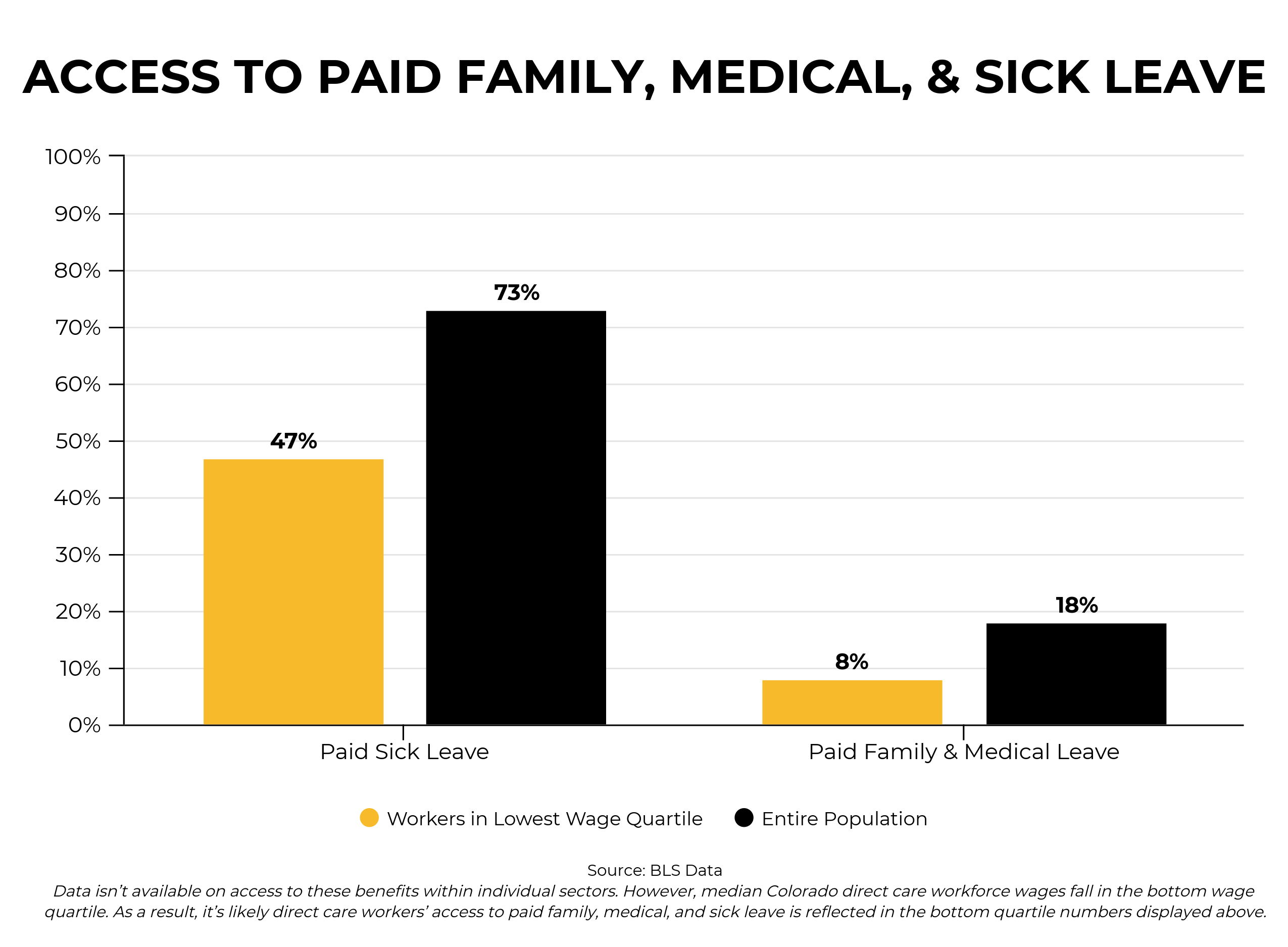
Without intervention, this preexisting lack of essential benefits keeps direct care workers from getting tested and treated for COVID-19 and, at best, makes it economically challenging for those who are sick (or potentially sick) to self-isolate. All of this at a time when it’s imperative for people to get treated and avoid contact with others when ill — especially if they’re likely to interact with our most vulnerable community members.
Emergency state and federal rules were recently passed to provide paid family, medical, and sick leave, as well as COVID-19-specific health coverage. An important first step, but there are still gaps in these provisions. New health coverage regulations cover testing, but not necessarily treatment — a potentially significant expense. Similarly, emergency paid leave regulations leave open the possibility for excluding health care workers from benefit eligibility.
Affordable Child Care Services
According to Bell analysis of IPUMS data, over 40 percent of direct care workers in Colorado have at least one child living with them, and 14 percent having a child under 5. As we’ve documented, child care costs for these and other low-income families were often already prohibitively expensive. However, as a result of COVID-19, widespread school closures have taken away an important source of child care for many employees, including direct care workers who don’t have the luxury of working from home.
To address these immediate and emergency needs, Governor Polis — with support from the state and federal government, as well as charitable institutions — has set up emergency child care for those providing essential services, including those working in long-term care facility settings. Free through May 17th, these services will be important throughout the entirety of this crisis.
Training & Resources
A lack of adequate training and resources explains part of the ongoing struggle to recruit and retain enough direct care workers. Problematic at the best of times, these challenges are clearly exacerbated under current circumstances. Workers across the country continue to voice concerns about the lack of adequate protective equipment and guidance on care techniques. The recently passed Coronavirus Aid, Relief, and Economic Security (CARES) Act provides for additional training and supplies for health care workers, including those in the direct care workforce. However, as the epidemic spreads, this support must be maintained.
Looking Forward
COVID-19 has exposed both the importance of direct care workers and the underlying flaws in how we support these individuals. On a daily basis, we’re witnessing what happens when the workers responsible for the care of our most vulnerable don’t have access to health and paid leave benefits, can’t afford essential services like child care, and lack quality training.
Emergency state and federal measures are helping to temporarily address gaps in the support system for direct care workers. But at some point, we’ll move beyond the public health emergency that is COVID-19. Even after this happens however, the underlying need to create a stronger direct care workforce will remain. As we look toward the future, it’ll be incumbent upon us to learn from this crisis, truly understand the value of our direct care workforce, and enact permanent measures to support these workers and those they care for.
